Infection control policies in UK care homes are robust, well-documented and closely aligned with national guidance. Yet in practice, the challenge for senior leaders is no longer knowing what good infection control looks like, but ensuring it is delivered consistently, across every shift, role and setting. This gap between policy and practice presents differently in residential and nursing homes, and closing it requires tailored approaches rather than one-size-fits-all solutions…
Residential homes: consistency in everyday care
In residential settings, infection control is most vulnerable during routine, high-volume interactions: personal care, communal dining, shared activities and environmental cleaning. While residents may have lower clinical acuity, the density of social contact increases transmission risk.
Best practice focuses on embedding infection control into daily routines, rather than treating it as a clinical overlay. This includes clear hand hygiene cues at points of care, simplified PPE protocols that reduce confusion, and cleaning schedules that align with how spaces are actually used, not how they are described in policy documents.
Training is most effective when it is practical, visual and repetitive. Short, role-specific refreshers delivered on shift, supported by peer champions, outperform annual classroom sessions. Senior leaders play a critical role by reinforcing expectations through visible behaviours, not just audits.
Nursing homes: managing complexity without overload
Nursing homes face additional challenges: invasive procedures, wound care, medical devices and higher resident vulnerability. Here, the risk is not a lack of policy, but cognitive overload: too many protocols competing for attention in high-pressure environments.
The best-performing nursing homes are streamlining guidance into clear, prioritised workflows. Visual checklists, standardised equipment layouts and clear escalation triggers help staff make the right decisions quickly. Infection control teams increasingly work alongside nursing leads to integrate prevention measures into clinical pathways rather than layering them on top.
Agency and bank staff remain a pressure point. Homes that manage this well provide rapid, standardised infection control induction supported by digital tools and clear accountability from shift leads.
Culture, not compliance
Across both settings, the most significant differentiator is culture. Staff are far more likely to follow infection control practices when they feel supported rather than policed. Open reporting of near misses, non-punitive responses to errors, and shared problem-solving all contribute to safer practice.
Importantly, senior leaders must recognise the operational realities staff face. Infection control measures that slow care delivery or add unnecessary steps are unlikely to be sustained, no matter how well intentioned.
Closing the gap
Effective infection control in care homes is less about introducing new policies and more about designing systems that work in real conditions. Residential and nursing homes may face different risks, but both benefit from the same principle: infection control succeeds when it is practical, prioritised and owned by everyone.
Are you searching for Infection Control solutions for your organisation? The Care Forum can help!
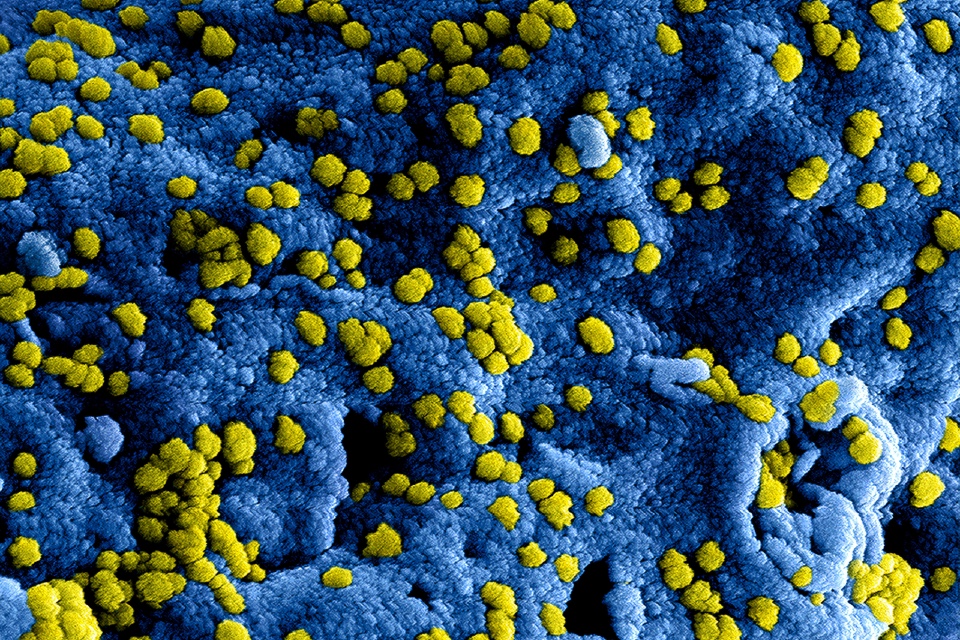
Photo by Vitaly Gariev on Unsplash